By Cecile Mantovani and Gabrielle Tétrault-Farber
LAUSANNE, Switzerland (Reuters) – A long-term Parkinson’s disease patient, Marc Gauthier had essentially been confined to his home until he became the first person to receive a new Swiss-designed implant that dramatically improved his ability to walk.
Gauthier, 63, received a neuroprosthetic at Lausanne University Hospital (CHUV), comprising an electrode field placed against his spinal cord. Combined with an electrical impulse generator under the skin of his abdomen, the device stimulates his spinal cord to activate his leg muscles.
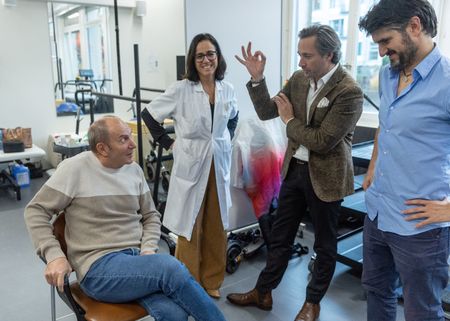
“It changed my life because I’m now independent,” said Gauthier, a native of the French city of Bordeaux, as he sat with his doctors at CHUV. “I can leave my home, run errands. I even go on foot.”
Parkinson’s is a degenerative neurological disease characterized by symptoms such as tremors, stiffness, and difficulty with balance and coordination.
The incidence of this disease has doubled over the past 25 years, according to the World Health Organization. Global estimates showed that more than 8.5 million people suffered from the disease in 2019.
Grégoire Courtine, one of the doctors leading the project, said the electrical pulses delivered to Gauthier’s spinal cord enabled him to walk the way he would have without the disease.
“We strongly believe that many individuals could benefit from this therapy,” said Courtine, a professor of neuroscience at the Swiss Federal Institute of Technology Lausanne (EPFL), the University of Lausanne and CHUV.
Published in the Nature Medicine journal on Monday, the findings by Courtine team’s at the NeuroRestore research centre suggest the technology could be used more widely in patients with advanced Parkinson’s, most of whom suffer from debilitating mobility issues.
Dave Marver, chief executive officer of Onward Medical, which designed the implant, said that while the device was similar to implantable defibrillators and devices used for pain management, it was unique in its in ability to target the spinal cord in a specific and flexible way.
“For the health care system, it will look and feel familiar, but it will offer therapy that doesn’t exist today,” he said.
Courtine’s team plans to carry out clinical tests on six new patients next year.
“With this therapy, if people can gain more confidence and can go out, have better social interactions and do more things, it’s an enormous plus in their daily activities and quality of life,” said Jocelyne Bloch, the neurosurgeon who carried out the surgery on Gauthier and a co-director of NeuroRestore.
(Reporting by Gabrielle Tétrault-Farber, Cécile Mantovani and Denis Balibouse; Editing by Bernadette Baum)